
Background: Recent advances in the treatment of myelodysplastic syndrome (MDS) have improved patient survival and quality of life (QOL), while reducing transfusion burden. However, allogeneic hematopoietic cell transplantation (HCT), widely used in younger MDS patients, remains the only curative therapy for MDS. While transplantation outcomes among selected older patients with MDS are similar to younger patients with MDS, early transplantation for older patients is infrequently offered since the relative benefits of HCT over non-HCT therapy in have not been well defined in this patient group. We conducted a multi-center, biologic assignment trial in older individuals with high risk MDS to define the benefit of HCT over non-HCT therapy.
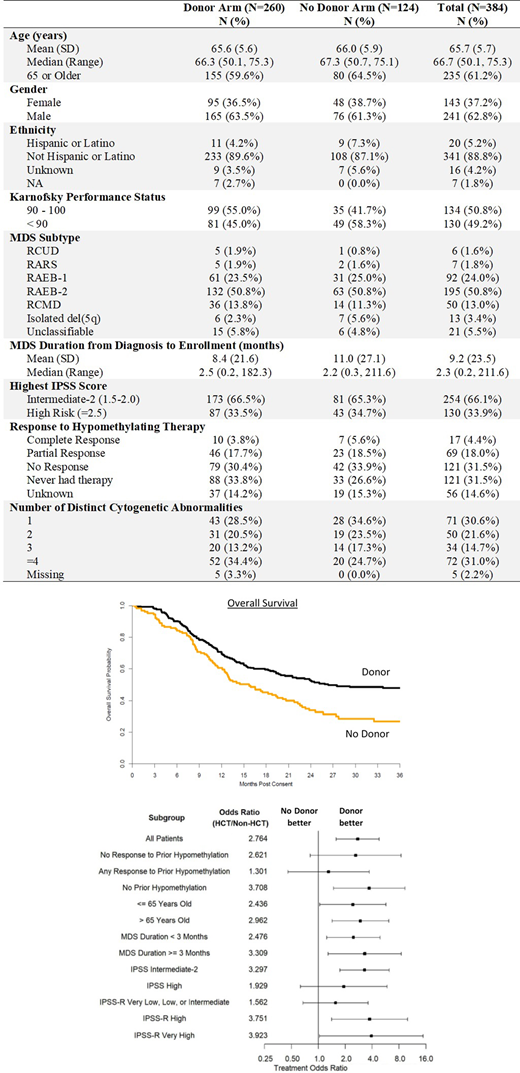
Methods: The study was a multicenter, biologic assignment trial in subjects aged 50-75 with higher risk de novo MDS (IPSS Intermediate-2 (Int-2) or High) who were candidates for reduced-intensity conditioning (RIC) allogeneic HCT, comparing outcomes of those with a suitable 8/8 HLA-matched donor to those without a donor. The trial was conducted by the Blood and Marrow Transplant Clinical Trials Network (BMT CTN 1102, NCT02016781). Eligible subjects were enrolled prior to a formal donor search, and before or after MDS treatment was initiated. Biological assignment to the Donor or No Donor arm was based on high-resolution HLA typing of eligible family members and a search of the unrelated donor registries. Subjects were initially assigned to the No Donor arm and re-assigned to the Donor arm when a suitable donor was identified. Subjects who died or whose 90-day donor search ended without identifying a suitable donor remained in the No Donor arm. Subjects in the Donor arm were expected to undergo RIC HCT within 6 months of enrollment. Subjects underwent RIC HCT or non-HCT therapy according to institutional standards. The primary analysis compared three-year overall survival (OS) between arms using adjusted survival estimates to account for the potential bias resulting from biological assignment. The sample size was selected to provide at least 80% power to detect a difference of 15% in 3-year OS. Between January 2014 and November 2018, 384 subjects (Donor n=260, No Donor n=124) were enrolled at 34 centers. The study arms were well balanced for age, gender, KPS, IPSS risk, MDS disease duration and responsiveness to hypomethylating therapy (Table). The median follow-up time for surviving patients was 34.2 months (range: 2.3-38 months) in the Donor arm and 26.9 months (range: 2.4-37.2 months) in the No Donor arm.
Results: In an intent-to-treat analysis, adjusted OS at 3 years from study enrollment in the Donor arm was 47.9% (95% CI: 41.3%-54.1%) compared with 26.6% (95% CI: 18.4%-35.6%) in the No Donor arm (p=0.0001, absolute difference 21.3%, 95% CI: 10.2%-31.8%)(Figure). A sensitivity analysis excluding subjects assigned to the No Donor arm who died or withdrew prior to the end of the 90-day search window showed no effect on outcome (Adjusted OS: 48.0% vs. 28.1%, p=0.0004). Leukemia-free survival (LFS) at 3 years was greater in the Donor arm (35.8%, 95% CI: 29.8%-41.8%) compared with the No Donor arm (20.6%, 95% CI: 13.3%-29.1%, p=0.003), with no changes in the sensitivity analysis. An OS and LFS benefit was seen across all subgroups tested (Figure).
There were no clinically significant differences in QOL between Donor and No Donor arms as measured by the FACT-G, the MOS-SF36 Physical and Mental Component Scores and the EQ-5D utility score at all time points.
The overall non-compliance rate for the trial was 26.3%. Reasons for non-compliance included the use of myeloablative conditioning or failure to proceed to RIC transplant in the Donor arm, and the use of alternative donors in the No Donor arm. In an as-treated analysis, comparison of the HCT and No HCT arms demonstrated a significant advantage in 3-year OS (47.4% vs. 16.0%, p<0.0001) and LFS (39.3% vs. 10.9%, p<0.0001) for subjects who underwent HCT.
Conclusions: We observed a significant OS advantage in older patients with Int-2 and High IPSS risk de novo MDS who are RIC HCT candidates and have an HLA-matched donor, when compared with those without a donor. The benefit of having a matched donor was seen across subgroups, including those who were of Medicare age (>65) and below. HCT should be offered to all individuals between the ages of 50-75 with Int-2 and High IPSS risk MDS in whom a suitable donor can be identified.
Nakamura:Magenta Therapeutics: Other: Advisory board meeting; Kyowa-Kirin: Other: Support on a meeting presentation; Alexion: Other: Support on a meeting presentation; Merck: Other: advisory board meeting; NapaJen Pharma: Consultancy; Kadmon Corporation: Other: Advisory board meeting; Celgene: Other: Support on seminar; Viracor: Consultancy. Scott:Alexion, Incyte, Novartis, Regeneron: Consultancy; Agios, BMS: Honoraria; BMS, Novartis: Research Funding. Oran:ASTEX: Research Funding; Celgene: Consultancy; Arog Pharmaceuticals: Research Funding. Maziarz:Novartis, Incyte, CRISPR Therapeutics, Artiva Biotherapeutics, and AlloVir: Consultancy; Novartis and Athersys: Other: DSMB participant; Athersys: Patents & Royalties; Incyte, Kite, BMS/Celgene, PACT Pharma, Orca BioSystems, and Omeros: Honoraria; Novartis and Juno: Research Funding. McGuirk:Allo Vir: Consultancy, Honoraria, Research Funding; Gamida Cell: Research Funding; Pluristem Ltd: Research Funding; Bellicum Pharmaceutical: Research Funding; Astellas: Research Funding; Fresenius Biotech: Research Funding; Novartis: Research Funding; Kite Pharmaceuticals: Consultancy, Honoraria, Research Funding, Speakers Bureau; Juno Therapeutics: Consultancy, Honoraria, Research Funding. Sekeres:BMS: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda/Millenium: Consultancy, Membership on an entity's Board of Directors or advisory committees. Cutler:Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees; Kadmon: Consultancy, Membership on an entity's Board of Directors or advisory committees; Jazz: Consultancy, Membership on an entity's Board of Directors or advisory committees; Medsenic: Consultancy, Membership on an entity's Board of Directors or advisory committees; Generon: Consultancy, Membership on an entity's Board of Directors or advisory committees; Mesoblast: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal